Chronic Thromboembolic
Pulmonary Hypertension
Chronic Thromboembolic
Pulmonary Hypertension
Incidence and Prevalence of Chronic Thromboembolic Pulmonary Hypertension
Incidence and prevalence of Chronic Thromboembolic Pulmonary Hypertension are reported to be 2–6 and 26–38 cases/million adults, respectively1,2,8,9
Very Common
PH associated with left heart disease [WHO Group 2]
Common
PH associated with lung disease [WHO Group 3]
Rare
- Pulmonary Arterial Hypertension [WHO Group 1]
- PH associated with pulmonary artery obstructions [WHO Group 4]
- PH with unclear and/or multifactorial mechanisms [WHO Group 5]
Pulmonary Hypertension is categorized into five groups according to the World Health Organization [WHO] classification
Group 1
PAH
Incidence and prevalence are reported to be ~6 and 48–55 cases/million adults, respectively.1,2 Idiopathic PAH is the most common subtype (50–60% of all cases), followed by PAH associated with connective tissue disease, congenital heart disease, and portal hypertension.1,3
Group 2
PH associated with left-sided heart disease
The prevalence of PH increases with severity of left-sided valvular diseases and can be found in 60–70% of patients with severe and symptomatic mitral valve disease4 and in up to 50% of those with symptomatic aortic stenosis.1,5
Group 3
PH associated with lung disease and/or hypoxia
~1–5% of patients with advanced COPD have an mPAP > 35–40 mmHg.1,6,7 8–15% of patients with idiopathic pulmonary fibrosis have an mPAP ≥ 25 mmHg, with prevalence increasing in advanced (30–50%) and end-stage disease (60%).1,7
Group 4
PH associated with chronic pulmonary artery obstruction
Incidence and prevalence of Chronic Thromboembolic Pulmonary Hypertension are reported to be 2–6 and 26–38 cases/million adults, respectively.1,2,8,9
Group 5
PH with unclear and/or multifactorial mechanisms
As the causes of this disorder are often multifactorial and can be secondary to increased pre- and post-capillary pressure, the incidence and prevalence in most cases are unknown.1
COPD, Chronic Obstructive Pulmonary Disease; mPAP, Mean Pulmonary Arterial Pressure; PAH, Pulmonary Arterial Hypertension; PH, Pulmonary Hypertension; WHO, World Health Organization.
References: 1. Humbert M, et al. Eur Heart J. 2022;43(38):3618–731. 2. Leber L, et al. Pulm Circ. 2021;11:2045894020977300. 3. Lau EMT, et al. Nat Rev Cardiol. 2017;14:603–14. 4. Tichelbacker T, et al. Herz. 2019;44:491–501. 5. Weber L, et al. Eur J Heart Fail. 2019;21:172–81. 6. Hurdman J, et al. Eur Respir J. 2013;41:1292–301. 7. Nathan SD, et al. Eur Respir J. 2019;53:1801914. 8. Delcroix M, et al. Eur Respir J. 2021;57:2002828. 9. Kramm T, et al. Clin Res Cardiol. 2018;107:548–53.
What is Chronic Thromboembolic Pulmonary Hypertension?
- CTEPH is defined as elevated pressure in the pulmonary artery (mPAP > 20 mmHg, PAWP ≤ 15 mmHg, and PVR > 2 WU) with persistent pulmonary perfusion defects as per the European Society of Cardiology/European Respiratory Society guidelines1
- While there is good evidence to support the recent change in mPAP threshold from ≥ 25 mmHg to > 20 mmHg in PH, the consequences for CTEPH are not yet established2
- Incomplete resolution and organization of thrombus after acute Pulmonary Embolism (PE) is a common cause of CTEPH3,4
- CTEPH is caused by fibrothrombotic vascular obstruction of the large pulmonary arteries and remodeling of small distal pulmonary arteries3. The extent of vascular obstruction is a major determinant of the severity of PH in patients with CTEPH1,5
- The US CTEPH registry reported that many patients with CTEPH (88%) had a history of acute PE with (46%) or without (42%) deep vein thrombosis6
- Worsening of PH may involve recurrent thromboembolism or in-situ thrombosis, and remodeling of small distal pulmonary arteries in the non-occluded areas, similar to that encountered in PAH5
- It is important to note that the absence of venous thromboembolism does not rule out CTEPH. Some patients with CTEPH report no history of PE (9–67%)2,6–9 or a history of deep vein thrombosis without PE (3%)4
CTEPH, Chronic Thromboembolic Pulmonary Hypertension; CTPA, Computed Tomography Pulmonary Angioplasty; PE, Pulmonary Embolism; sPAP, Systolic Pulmonary Arterial Pressure.
References: 1. Humbert M, et al. Eur Heart J. 2022;43(38):3618–731. 2. Kim HN, et al. ERJ. 2019;53:1801915. 3. Boon G, et al. Res Pract Thromb Haemost. 2020;4(6):958–68. 4. Lang I, et al. Eur Respir J. 2013;41:462–8. 5. Dartevelle P, et al. Eur Respir J. 2004;23:637–48. 6. Kerr KM, et al. CHEST. 2021;160(5):1822–31. 7. Pepke-Zaba J, et al. Circulation. 2011;124:1973–81. 8. Tanabe N, et al. Intractable Disease Database. 2008. 9. Gall H, et al. Eur Respir Rev. 2017;26:160121.
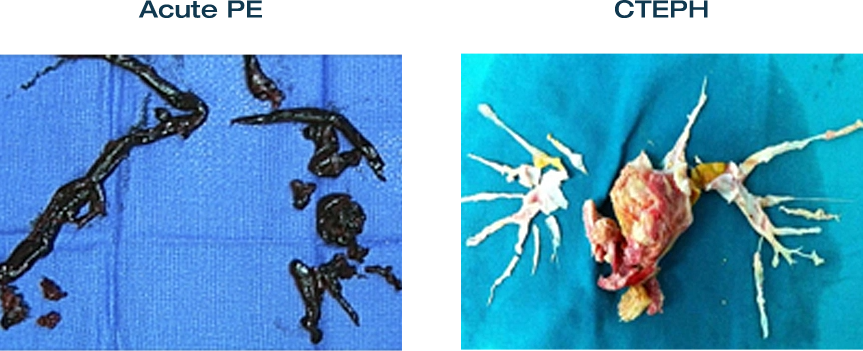
Photos used courtesy of Prof B Yildizeli, Marmara University Hospital, Turkey.
CTEPH should be considered after PE if:
- Radiology signs suggest CTEPH on the CTPA performed to diagnose PE
- Estimated sPAP is > 60 mmHg on echocardiogram
- Dyspnea or functional limitations persist in the clinical course post-PE
- Asymptomatic patients have risk factors for CTEPH or a high CTEPH predication score
Reference: Humbert M, et al. Eur Heart J. 2022;43(38):3618–731.
CTEPH: Mechanisms of Small-Vessel Disease
Three mechanisms contribute to small-vessel disease in CTEPH, which may occur alone or in combination:

IPAH, Idiopathic Pulmonary Arterial Hypertension.
Reference: Galiè N and Kim NH. Proc Am Thorac Soc. 2006;3:571–6.
Chronic Thromboembolic Pulmonary Hypertension versus Pulmonary Arterial Hypertension

BPA, Balloon Pulmonary Angioplasty; CT, Computed Tomography; MRI, Magnetic Resonance Imaging; NO, Nitric Oxide; PE, Pulmonary Embolism; V/Q, Ventilation Perfusion.
References: 1. Humbert M. Eur Respir Rev. 2010;19:59–63. 2. Humbert M, et al. Eur Heart J. 2022;43(38):3618–731. 3. Keogh AM, et al. J Am Coll Cardiol. 2009;54:S67–77. 4. Kim NH, et al. J Am Coll Cardiol. 2013;62:D92–9.
Diagnosis of CTEPH
Ventilation/perfusion (V/Q) scintigraphy is the diagnostic test of choice for CTEPH screening1
- A normal V/Q scan can exclude CTEPH with a sensitivity of 96–100% and a specificity of 90–95%2-4
- If mismatched perfusion defects are detected, diagnosis of CTEPH should be confirmed using RHC and pulmonary angiography1
Computed tomography pulmonary angiography can also be used to detect direct or indirect signs of CTEPH5
- Diagnostic accuracy is more limited with a sensitivity and specificity of 76% and 96%, respectively1,6
- Chronic thrombi are visible as bands, webs, stenoses, and occlusions5

CTEPH, Chronic Thromboembolic Pulmonary Hypertension; CTPA, Computed Tomography Pulmonary Angiography; DSA, Digital Subtraction Angiography; PE, Pulmonary Embolism; PH, Pulmonary Hypertension; RHC, Right Heart Catheterization; V/Q, Ventilation Perfusion.
References: 1. Humbert M, et al. Eur Heart J 2022;43(38):3618–731. 2. Kligerman S and Hsiao A. Pulm Circ 2021;11(2):1–12. 3. He J, et al. Nucl Med Commun 2012;33:459–63. 4. Tunariu N, et al. J Nucl Med 2007;48:680–4. 5. Boon G, et al. Res Pract Thromb Haemost 2020;4(6):958–68. 6. Dong C, et al. PLoS One 2015;10:e0126985.
Treatment of CTEPH
- Patients with confirmed Chronic Thromboembolic Pulmonary Hypertension (CTEPH) must undergo an operability assessment at expert surgical CTEPH center to determine whether they are candidates for first-line, potentially curative surgery: pulmonary endarterectomy
- Dependent on the outcomes of the operability assessment, the recommended treatment for CTEPH is lifelong anticoagulation therapy and a multimodal approach of combinations of pulmonary endarterectomy, balloon pulmonary angioplasty, and medical therapies to target mixed anatomical lesions
BPA, Balloon Pulmonary Angioplasty; CTEPH, Chronic Thromboembolic Pulmonary Hypertension; MDT, Multidisciplinary Team; PEA, Pulmonary Endarterectomy; PH, Pulmonary Hypertension; sGC, soluble guanylate cyclase; WHO FC, World Health Organization Functional Class.
Reference: Humbert M, et al. Eur Heart J. 2022;43(38):3618–731.